PMDD: A Life-Threatening Mental Illness
Getting my period is sweet, sweet psychological relief — and not because I'm avoiding pregnancy.
The beginning of menstruation for me marks the end of the worst phase of my cycle.

My illness gave me a 1 in 3 chance of a suicide attempt before age 45 — and about 14 years of suffering before getting a proper diagnosis. Even within my lifetime, professionals hotly debated whether my condition was "real."
Despite what American media may have told you, menstrual cycles are so much more than "bleeding" and "not bleeding."
I've heard the sentiment echoed repeatedly: my friends with PMDD (the worst PMS) and I generally experience symptoms a week or two before the period starts. The delay may make it harder to pinpoint what's going on, but learning the differences among each phase has made all the difference in managing my mental health.
I finally went on intermittent medication for PMDD in early 2020.
Immediately after ovulation, I started two weeks of fluoxetine, then took two or three weeks off once my period started, and repeated. Most people haven't heard of such a schedule for SSRI usage, but it was changed my life — a year that sucked in so many ways turned out to be of the best times for my mental health.
Negative thoughts slipped off of me like I was Teflon. And that was all made possible by 7 little pills every month.
2025 UPDATE: Nowadays, it's just the occasional escitalopram here and there when I need it. Otherwise, hypnosis and having a flexible work schedule that allows for ample self-care managed most of my PMDD. I'm doing surprisingly well, for hardly taking meds — just vibing over here!
While the battle is over for me, the war isn't over for the AFAB (Assigned Female At Birth) people with premenstrual dysphoria disorder. Let's destigmatize hormone-related mental illness.
- I. What is it like to have premenstrual dysphoria disorder (PMDD)?
- II. What causes PMDD? (And what is it not?)
- III. How do I know if my depression is actually PMDD or PME?
- IV. Why might it take someone a long time to get a PMDD diagnosis and treatment?
- V. Taking medicine for premenstrual dysphoria: my experience
- VI. The end of my internal war? Well, yes, but actually, no!
- VII. PMDD was and still is a highly misunderstood condition.
- VIII. If you found this post helpful, consider leaving me a tip!
Disclaimer
This blog post isn't meant to be an end-all resource but to talk about my personal experience with premenstrual dysphoria.
What is it like to have premenstrual dysphoria disorder (PMDD)?
Content warning: depression, suicidal ideation, menstruation
In the simplest terms, PMDD (short for premenstrual dysphoria disorder) is like PMS on steroids, but I also don't think that description does justice to how severe it is.
PMDD for me used to mean being practically bedridden for half of every month
Every visceral sensation that stirred up:
- My worst, most traumatic memories
- The times other people screwed me over
- The times I screwed others over
- Every worry about whether my existence burdened others
…inhabited my body, rent-free. I intellectually knew that the threats were gone, but the physiology behind the knot in my chest, the throat constriction, and the fire in my face and ears was all real.
Even when my life was otherwise going well, the flashbacks haunted me, like Black Mirror-esque augmented reality using my brain against me.
It was a mix of debilitating depression, OCD, and anxiety:
- What if I give in to my rage?
- What if I snap at my boss or my partner?
- What if my pain leads me to actions that alienate the ones I love?
- What if those ghosts in my past were right, and everyone around merely tolerates me?
It was like living half a life.
During one half, it was hard enough to survive — let alone hold down a "normal" job. Basic self-care felt like training in a gym one day and suddenly being launched into the Hunger Games the next. The other half felt like constantly cleaning up messes and playing catch-up.
What causes PMDD? (And what is it not?)
Premenstrual dysphoria disorder is a heritable, abnormal response to normal hormone fluctuations.
The current conceptualization is that someone can have normal progesterone levels but still have low levels of its metabolite, allopregnanolone, leading to low serotonin. And that's actually part of why fluoxetine works at lower doses and more quickly for PMDD than for "traditional" depression: the target is short-term allopregnanolone increase rather than long-term selective serotonin reuptake inhibition.
Either way, PMDD is not always the same thing as having a hormonal imbalance, though that can certainly make PMS worse! If you have PMDD, it may also be harder to foster optimal hormonal health by adjusting eating habits, sleeping hygiene, and exercising alone.
I also want to be clear that PMDD is a disorder.
Something is wrong with my hormone receptors, but that doesn't apply to people with uteruses who have symptom-free cycles or only mild PMS symptoms. PMDD affects about 5.5% of AFAB people.
Furthermore, while there's much overlap between PMDD and depression, they're not exactly the same thing. Teasing apart the differences between the two means you can find a treatment plan that works better for you.
How do I know if my depression is actually PMDD or PME?
Get to know your body and track your cycles and symptoms for at least two months.
Ideally log for longer than that, if you can. Discern the phases of your cycle:
- Menstrual phase — the actual period
- Follicular phase — estrogen rises as the egg prepares to be released
- Ovulation phase — the most fertile phase; estrogen peaks
- Luteal phase — progesterone rises as the body prepares for potential pregnancy
There are articles galore online about tracking your cycle, usually in the context of conception. If you want a more in-depth book, Wild Power and Taking Charge of Your Fertility are great starting points. The former is woo-woo but a super useful field guide to the cyclical fluctuations, based on how they feel spiritually and emotionally. The latter goes into detail about observable body temperature changes and cervical mucus.
Take the GAD‑7 and PHQ‑9 inventories every week.
They're questionnaires for determining how severe someone's anxiety and depression symptoms are, respectively.
If your depression or anxiety happens pretty much only after ovulation and before menstruation, you may have PMDD. There are different levels to it, though — for some, symptoms disappear when their periods arrive. For others, they continue to linger. If you have symptoms throughout your cycle, but they get worse during the luteal phase, you may have PME (premenstrual exacerbation) of another mental illness.
In any case, it's all good information to note for your treatment plan.
More clues to figure out which menstrual cycle phase you're in
For me, it's mostly about the lower abdominal sensations.
I feel sharp, focused, needle-like cramps on one side at a time during ovulation. That's my cue to start my medicine — before I feel the dull, centered cramping of my endometrium building up. There's usually a week of that before the pain intensifies and gets jabbier for a few days, and then my period starts.
I also notice more subtle changes in my habits
OOH LORDT, the changes aren't subtle anymore. I NOTICE them.
During ovulation, I display more energetic and manic-like (read: frisky) behavior. I'm also more excited about stereotypically Aphrodisian and feminine delights, like sex toys, lingerie, and makeup. During my luteal (a.k.a. depressive) stage, I used to feel inclined to listen to sad music, e.g. Deliverance by CHVRCHES on repeat.
With proper PMDD management — and Wild Power's insights — I've come to appreciate that my luteal phase doesn't have to be all bad. It could be considered more chill, or more focused on different, deeper, more spiritual behind-the-scenes work. I'm more receptive to intuitive insights when meditating and what's wrong with being sensitive, anyway? I felt flooded with joy watching The Wild Robot.
Why might it take someone a long time to get a PMDD diagnosis and treatment?
Simply put, I didn't know what I didn't know. Multiple reasons accumulated for me personally:
1. I got my first period at 11; nobody in my life considered that a pre-teen could have hormone-related issues.
2. My depressive symptoms were chalked up to "just" being a moody and difficult adolescent.
3. The worst part was about 10 days before my period, so I didn't think to link the two at first. Not when our media frames female anger as, "ArE yOu oN yOuR pErIoD?" PMDD is quite a bit before that; I feel better as soon as my period starts.
4. During my good phases, it was too dang easy to forget just how bad things were before
5. I was scared of possible side effects from birth control or SSRIs.
6. I didn't think that intervention was necessary — surely I could bootstrap lifestyle changes and talk therapy, right?
What were the last straws for me?
I've tried to manage my mental illness through supplements, journaling, yogic meditation, exercise, dietary adjustments — you name it. I'm a self-improvement junkie. If my knowledge about those things could have worked for me at the time, it would have.
Ultimately, I decided that, regardless of whether I did everything "perfectly," I didn't deserve to feel like shit. I could take medicine and work hard to maintain a healthy lifestyle and not want to die!
Imagine someone had high cholesterol due to genetics, and a doctor thought that medicine would greatly increase their quality of life and lower their risk of early death. Many people would go for it! But our culture doesn't give mental health care the same gravitas.
Another piece is that, while talk therapy stabilized me in acute crisis, it didn't help me build long-term coping mechanisms. Even when I talked through one issue and "got over" it, my low-serotonin brain would find something else to freak about.
And again, even when my life was great, I'd end up freaking out about freaking out.
It actually helped me out a lot when a counselor outright told me, "PMDD is outside the realm of what I can help you with." It prompted me to seek the right practitioners for the job: a gynecologist, a psychiatrist familiar with PMD, and therapists or coaches with experience in somatics.
Modalities that actually worked for me in the long term included hypnosis and EMDR.
It also felt so deeply affirming to hear a psychiatrist say things like:
- "Oh, wow. You're having a hard time."
- "I'm sure you've done your research."
That might sound basic, but when you're a woman of color, having a doctor take your illness seriously means the world. In some cases, it could be the difference between life and death.
Taking medicine for premenstrual dysphoria: my experience
I asked my gynecologist what the different treatment options were. They vary from case to case, but here's a quick summary of what to do if lifestyle changes alone aren't cutting it:
- Hormonal birth control
- An SSRI throughout the month
- An SSRI only during the luteal phase
I opted for the third option, starting with a tiny 5 mg dose of fluoxetine after ovulation, and pretty much immediately felt better. It was kind of wild to experience mild cramping but no moodiness whatsoever.
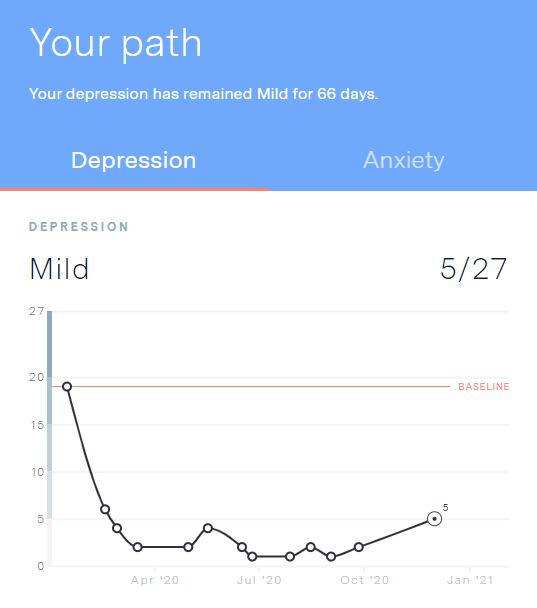
Take a look at my GAD‑7 and PHQ‑9 results from 2020.
I went from a 16/21 (moderate-severe) for anxiety and 19/27 (moderate) for depression down to a 3/21 and 6/27 during my first month of medicine alone.
Though the numbers fluctuate, they've at times been as low as 0 — no anxiety — and 1 for minimal depression. And bear in mind: that was all during the clusterfuck of 2020.

Most of my friends (taking SSRIs for "general" depression) told me that it would be weeks before much effect took place, but that wasn't the case for me. They also warned me of terrible withdrawal effects, and I didn't experience that, either.
Depressive symptoms may return if I miss a dose, but I can take a pill and feel better again within a matter of hours.
Why? Because women in their luteal phases are more sensitive to fluoxetine. In such cases, Prozac works by acting on allopregnanolone receptors rather than via the "conventional" way of selective serotonin reuptake inhibition over time.
And all those terrible sexual side effects people warned me about?
Nothing like that happened to me. They're real, but they don't affect everyone, and they're not the end of a great sex life.
That was… it? Had over a decade of suicidal thoughts and seeing red met their deus ex machina?
The end of my internal war? Well, yes, but actually, no!
The truth is that it took me a long internal battle before I tried medicine, and my qualms were valid.
I didn't have a good time with birth control (bye, libido!) or Celexa (hello, shit runs! I immediately stopped taking it) before, and I've been emotionally scalded by condescending doctors. One of them dismissed my concerns about sexual side effects and said, "The more you masturbate, the longer it takes to orgasm."
Nobody could blame me for proceeding with caution.
I recognize that what happened couldn't have been different. How could I have known what to do about premenstrual dysphoria disorder at 11, considering that a mere 5 years prior, there was a huge controversy about its validity, let alone medication for it?
And even then, I was lucky that the first antidepressant I took as an adult worked. Not everyone is as fortunate.
Ultimately, psychiatric medicine didn't make me happy, but it removed the biggest barrier. Now, I have a fighting chance.
PMDD was and still is a highly misunderstood condition.
Imagine you have head-splitting migraines, but you live in a world where not even half of the population has any form of headache at all. Those with mild head tension may think you're just dramatic and using your debilitating migraine as an excuse to be bitchy.
The stigma around PMDD is kind of like that. While I can't upheave that by myself, I hope this post helps others manage their mental health and remember that they're not alone. For further reading, check out the International Association for Premenstrual Disorders.
Do you or someone you know have severe PMS, PMD, or PME? How have you managed it?
If you found this post helpful, consider leaving me a tip!
- PayPal: supersmashcache@gmail.com
- Venmo: @supersmashcache
- Shop sex toys via my favorite online boutiques
Discover more from Super Smash Cache
Subscribe to get the latest posts sent to your email.











Thanks so much for sharing in depth about your experience with PMDD. It sounds like you've worked so incredibly hard to live with and manage this illness, and where you are now with it is truly hard-won 🥺
I think it's incredible you have been able to/worked to get yourself to a place to build a lifestyle around your bodymind's needs, esp with your work being flexible and sustainable enough to support you!
I was wondering:
1. Do you experience anxiety and OCD symptoms during the phase you experience your depressive symptoms?
2. Your 2023 update means you're no longer taking the fluoxetine, if I'm understanding correctly? Would you be open to sharing how you use hypnosis and EFT tapping as part of your care regimen? Do you use it specifically when you have symptoms? Or do you use it all throughout the month?
Thanks!
Hi, here's another update for 2024:
Here's a free sample library from Desiree Eckert: https://www.desmerized.com/microdose-archive
It's also available on Spotify under the podcast name, "Weekly Microdose of Hypnosis"
I didn't have PMDD, however I have major depressive disorder with anxiety and I had postpartum depression after my last child. I'm now in the middle of perimenopause, and it shocked me that without any other major change in my life, I was suddenly in a deep depressive episode with suicidal ideation. One day I just couldn't think straight, I couldn't function, and despite having a lot to live for, I just didn't want to exist anymore. What I didn't know is that anyone who has either a history of depression OR a history of PMDD or PPD (hormonal-related depression, is at a SIGNIFICANTLY higher risk for depression during perimenopause. Even my shrink and my psychologist didn't tell me! And they're women!
Every woman is at higher risk for depression during perimenopause or menopause, regardless of history, and the medical profession is trying to train gynecologists and PCPs to more regularly screen for depression during the early stages of perimenopause.
Thank you for bringing attention to PMDD. I've learned so much about my own depression as I cycled through meds and treatments that didn't work. Genetic testing for meds helped me a great deal (it's only done through a doctor, so the information is confidential, and it's nothing like the commercial genetic testing options). Therapy, sleeping regularly, eating regularly, and a support network helps. But I wouldn't be alive right now if I didn't have an excellent psychiatrist handling my meds. PCPs are not equipped to prescribe psychotropic meds, period. It's been 9 months and we're still working on the right med balance, because of how everything changed when my body shifted into another stage of peri.
You're not alone — and I'm grateful that you shared what you've been going through. I swear if men went through 1/100th of what we do, there'd be no issues with funding, research, and insurance coverage of psychological care.
Especially during Covid–where there's so much exacerbation and overlap of physical and emotional symptoms –this is really important information for people to have. I've always resisted the medications you mentioned out of fear of side effects, so it's good to know that those aren't a given…
Thank you for bringing attention to this life-threatening condition. All too frequently, doctors dismiss people who struggle with the psychological effects of hormone fluctuations as just being overly emotional. By writing about your experience you have likely helped a number of people realize that they should be taken seriously and that there are treatments available.
I had no idea that this was a thing. All I can really say is thank you for writing this
Wow. This is extremely informative. I had heard of PMDD before but didn't know the particulars. Thanks!
Thank you for writing this. I've have PMDD and went on birth control to manage the suicidal ideation I'd have about — you said it — ten days before my period. It was hell. I was taking all my bipolar meds but I was experiencing some of the worst depression of my life. I got scared that I'd act on the ideation so I went to my gyno and begged for relief.
She put me on hormonal birth control and holy hell did my life change (for the better). I could function again, I could live again, and I didn't have those thoughts anymore.
For me, I don't have a lot of physical pain. It's just a shitton of mental pain and instability. I'm so happy that the birth control worked for me.